Titin Myopathy and Titin Muscular Dystrophy:
Do YOU know the Difference?
By by Sarah Foye, Team Titin, Patrick Foye, M.D., Alan Beggs, PhD, Director, The Manton Center for Orphan Disease Research, Boston Children’s Hospital and Divya Jayaraman, MD, PhD, Boston Children’s Hospital.
Key points:
- “Myopathy” and “Muscular Dystrophy” are both medical terms that refer to problems with muscle function.
- There is significant overlap in meaning between these two terms, but also some differences.
- “Myopathy” refers to any muscle disorder, and includes muscular dystrophies.
- A muscular dystrophy is a particular type of myopathy where the muscle tends to break down over time.
- Myopathies may or may not have clinical worsening overtime, depending on the specific cause, type, presentation, etc.
Key points specifically regarding Titin:
- The TTN gene codes for the protein Titin, which is crucial for muscle function.
- Genetic mutations in the TTN gene can cause abnormalities in the Titin protein. This can cause either a (non-dystrophic) Titin Myopathy or a Titin Muscular Dystrophy, depending on the specific genetic mutation.
Explanation:
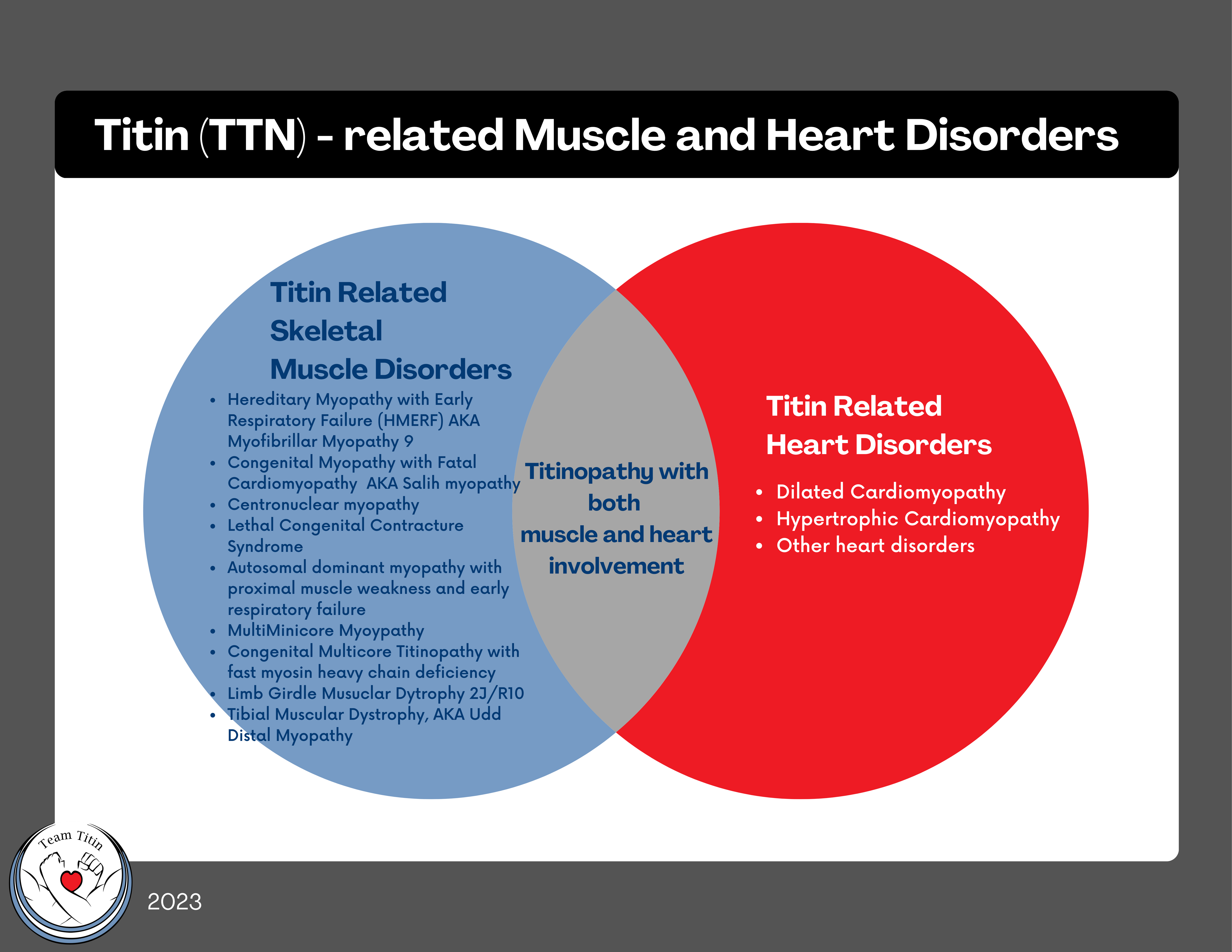
Changes in the titin (TTN) gene can cause a range of muscle disorders sometimes called:
- Titinopathy (any medical condition caused by an abnormality of titin)
- Titin myopathy (usually referring to less progressive weakness without significant muscle breakdown, or dystrophy)
- Titin Muscular Dystrophy (reserved for more progressive forms of titin-myopathy with evidence for muscle breakdown (dystrophy)
- There are many subtypes of Titinopathy, named based on particular prominent clinical or microscopic findings (see below)
Titin is a protein found in muscle tissue where it plays a crucial role in the function and structure of muscle fibers. Mutations in the TTN gene that codes for titin can lead to two different muscle disorders: a titin “myopathy” or a titin “muscular dystrophy”. Let’s consider the difference between them.
Myopathy:
If we look at the breakdown of the word “myopathy”: “myo ” means muscle and “pathos” means disease. A myopathy is literally a medical condition where the problem is at the muscle itself. This is an umbrella term that can refer to muscle diseases with a variety of causes including genetic mutations, infections, autoimmune disorders, and exposure to certain drugs or toxins. Our interest for this article focuses on titin-related myopathies, which are caused by genetic mutations in the titin (TTN) gene. Myopathies can be congenital (present at birth or early childhood) or acquired (developed later in life). Children who have symptoms at birth or in early childhood may be described as “congenital titinopathy” or “recessive titinopathy”.
Specific forms of titinopathy are often named based on the primary symptom, or appearance of the muscle under the microscope.
Some categories of myopathies that can be cause by titinopathy include:
- Hereditary Myopathy with Early Respiratory Failure (HMERF) also known as Myofibrillar Myopathy 9 or MFM-titinopathy
- Congenital Myopathy with Fatal Cardiomyopathy also known as Salih myopathy
- Centronuclear myopathy (CNM) related to TTN
- Lethal Congenital Contracture Syndrome
- Autosomal dominant myopathy with proximal muscle weakness and early respiratory failure
- MultiMinicore Myopathy (MmD) related to TTN
Dystrophy:
Muscular dystrophy is the general term for a group of muscle diseases (“myopathies”) condition marked by progressive (worsening) weakening and wasting of the muscles. For titin muscular dystrophy, this can result in the muscle cell not functioning properly. This can lead to instability, injury and breakdown. In healthy muscle, cells repair themselves but with muscular dystrophy the rate of damage can overwhelm or exhaust the repair process. This can lead to a breakdown of the muscle which is then replaced by scar and fatty tissues. Eventually, this will lead to muscle loss and progressive loss of function, accounting for why patients typically become weaker over time. Sometimes, byproducts of this breakdown leaks into the bloodstream and can be measured by a blood test. So, some people with muscular dystrophy may have elevated blood levels of creatine kinase (CK) released into the blood as muscle tissue is damaged. Dystrophic changes in the muscle could then be proven by:
1. Analysis of the muscle tissue under the microscope that shows evidence of fibrous or fatty replacement in the cell
2. Blood test that shows evidence of muscle breakdown
3. Muscle imaging studies such as ultrasound or MRI that show dystrophic changes in the muscle.
So, a titin muscular dystrophy is a an inherited disorder that results in progressive (worsening) muscle weakness and degeneration.
Some categories of muscular dystrophy that can be caused by titin mutations (titinopathies) include:
- Limb Girdle Muscular Dystrophy R10 – titin related (LGMDR10) also known as LGMD2J in the old naming system
- Tibial Muscular Dystrophy (2) also known as Udd Distal Myopathy or Udd distal myopathy – tibial muscular dystrophy (UDM-TMD), or Udd Myopathy
“The difference between congenital myopathies and muscular dystrophies is that dystrophies are gradually progressive [worsening] and are associated with increased muscle breakdown with age.” (1) So, a broad generalization would be that (non-dystrophic) myopathies are generally stable over time while muscular dystrophies have progressive (worsening) muscle breakdown over time.
To further confuse matters, some disease subtypes may be classified as a myopathy but sometimes present with dystrophic features, e.g. HMERF or tibial muscular dystrophy (2,3).
In general, congenital titinopathies with onset in childhood, tend to be more static in nature as far as functional status. Later onset titinopathies with symptoms starting in adulthood tend to be dystrophic and progressive (worsening) over time.
In summary, myopathy is an umbrella term that refers to muscle diseases of various causes. A titin-related myopathy means any muscle disease caused by a change in the titin (TTN) gene. A titin-related muscular dystrophy would refer to a muscle disease caused by a change in the titin (TTN) gene when there is evidence of worsening muscle breakdown with replacement by scar or fatty tissue.
- Pasrija D, Tadi P. Congenital Muscular Dystrophy. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558956/
- Udd B, Hackman P. Udd Distal Myopathy – Tibial Muscular Dystrophy. 2005 Feb 17 [updated 2020 Jan 2]. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2023. PMID: 20301498.
- Pfeffer G, Barresi R, Wilson IJ, Hardy SA, Griffin H, Hudson J, Elliott HR, Ramesh AV, Radunovic A, Winer JB, Vaidya S, Raman A, Busby M, Farrugia ME, Ming A, Everett C, Emsley HC, Horvath R, Straub V, Bushby K, Lochmüller H, Chinnery PF, Sarkozy A. Titin founder mutation is a common cause of myofibrillar myopathy with early respiratory failure. J Neurol Neurosurg Psychiatry. 2014 Mar;85(3):331-8. doi: 10.1136/jnnp-2012-304728. Epub 2013 Mar 13. PMID: 23486992; PMCID: PMC6558248.